Endodontic treatment, also known as root canal treatment, is a dental procedure that has been widely used to save teeth from extraction. It involves the diagnosis, treatment, and management of diseases affecting the dental pulp and tissues surrounding the roots of teeth. Understanding endodontic treatment is crucial for anyone experiencing dental pain or discomfort, as it offers an effective solution to alleviate symptoms and restore oral health. This article aims to provide a comprehensive guide to endodontic treatment, covering topics such as diagnosis, symptoms, causes, treatment options, procedures, and aftercare. By delving into each aspect, readers will gain a thorough understanding of endodontic treatment and be better equipped to make informed decisions regarding their dental health.
1. "Understanding Endodontic Treatment: Diagnosis and Symptoms"
Endodontic treatment, also known as root canal therapy, is a dental procedure performed to treat infected or damaged tooth pulp. This type of treatment is crucial for saving a tooth that would otherwise require extraction. Understanding the diagnosis and symptoms of endodontic treatment is essential in identifying the need for this procedure and seeking timely dental care.
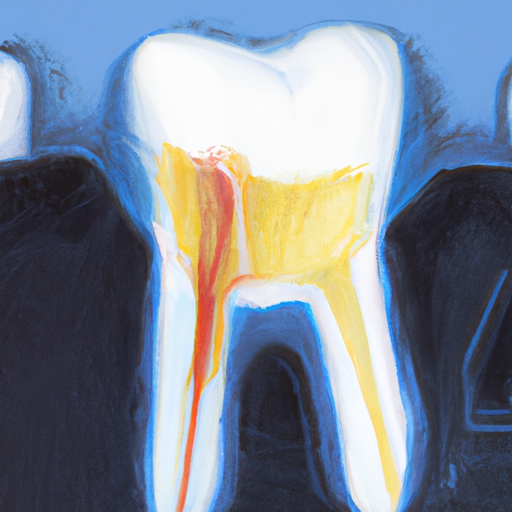
Diagnosis of endodontic treatment involves a comprehensive examination by a dentist or endodontist. The dentist will evaluate the patient’s dental history, perform a thorough clinical examination, and may order additional tests such as X-rays or pulp vitality tests. The goal is to identify any signs of infection or damage to the tooth’s pulp, which is the soft tissue inside the tooth that contains nerves, blood vessels, and connective tissue.
One of the primary symptoms that may indicate the need for endodontic treatment is persistent tooth pain. This pain can range from mild to severe and may be triggered by various stimuli such as hot or cold temperatures, chewing, or even just touching the affected tooth. Other symptoms include sensitivity to pressure, swelling around the affected area, and the presence of a small pimple-like bump on the gum near the tooth.
In some cases, the symptoms of endodontic problems may not be immediately apparent. This can occur when the infection or damage to the pulp is in its early stages or when the tooth has undergone trauma. Regular dental check-ups are crucial for early detection of such issues. Dentists are trained to identify subtle signs that may indicate the need for endodontic treatment before the symptoms worsen.
The causes of endodontic problems are varied but often result from tooth decay, deep cavities, cracks or fractures in the tooth, repeated dental procedures on the same tooth, or trauma to the tooth. When tooth decay or a cavity is left untreated, bacteria can penetrate the tooth’s outer layers and reach the pulp, leading to infection and inflammation. Similarly, cracks or fractures in the tooth can provide an entry point for bacteria, causing pulp damage.
It is important to note that endodontic treatment
2. "Exploring the Causes of Endodontic Issues and Treatment Options"
Endodontic issues, also known as root canal problems, can be caused by a variety of factors. Understanding the causes of these issues is crucial in determining the appropriate treatment options.
One common cause of endodontic problems is dental decay or cavities. When tooth decay progresses to the point where it reaches the pulp, which contains nerves and blood vessels, it can lead to infection and inflammation. This infection can spread to the surrounding tissues, causing pain and discomfort.
Another cause of endodontic issues is dental trauma. Trauma to the tooth, such as a sports injury or accident, can damage the pulp and result in inflammation or infection. Fractures or cracks in the tooth can also allow bacteria to enter the pulp, leading to similar complications.
Poor oral hygiene practices can contribute to the development of endodontic problems. Inadequate brushing and flossing can lead to the buildup of plaque and tartar, which harbor harmful bacteria. Over time, these bacteria can penetrate the tooth and cause infection in the pulp.
Additionally, certain dental procedures can increase the risk of endodontic issues. For example, repeated dental treatments or restorations on a tooth can weaken the tooth structure and make it more susceptible to infection. Similarly, extensive dental work, such as multiple fillings or crowns, can cause stress on the tooth and potentially damage the pulp.
When it comes to treating endodontic issues, the most common approach is root canal therapy. This procedure involves removing the infected or inflamed pulp from the tooth, cleaning and disinfecting the root canals, and then filling and sealing them. Root canal therapy aims to save the natural tooth by eliminating the infection and preventing further damage.
In some cases, however, root canal therapy may not be sufficient to address the problem. If the tooth is severely damaged or the infection is extensive, endodontic surgery, such as an apicoectomy, may be necessary. This procedure involves removing the tip of the tooth’s root and any infected tissue surrounding it.
If the tooth is beyond repair
3. "Comprehensive Guide to Endodontic Treatment: Diagnosis, Procedures, and Aftercare"
Endodontic treatment, also known as root canal treatment, is a dental procedure that involves the diagnosis and treatment of issues affecting the inside of a tooth. This comprehensive guide aims to provide a detailed overview of endodontic treatment, including the diagnosis process, the procedures involved, and the essential aftercare steps for optimal recovery.
Diagnosis is the first crucial step in endodontic treatment. Dentists typically identify the need for root canal therapy through various symptoms and diagnostic tools. Patients may experience persistent tooth pain, sensitivity to hot or cold temperatures, swelling, or tenderness in the surrounding gums. X-rays, pulp tests, and careful examination of the affected tooth help dentists determine if endodontic treatment is necessary.
Once the diagnosis is confirmed, the procedure begins with the administration of local anesthesia to ensure the patient’s comfort. The dentist then creates an access point by drilling a small hole in the tooth to reach the infected or damaged pulp inside. The infected pulp is carefully removed, and the root canals are thoroughly cleaned and shaped using specialized tools. This step ensures the complete removal of any bacteria, debris, or infected tissue.
After cleaning the root canals, the dentist fills them with a biocompatible material called gutta-percha. This material seals the canals, preventing reinfection and restoring the tooth’s structural integrity. In some cases, the dentist may delay the placement of the permanent filling material to allow time for the tooth to heal completely.
Following the completion of the endodontic procedure, the tooth may require a dental crown or filling to provide additional protection and support. The crown or filling helps restore the tooth’s functionality and prevents any future damage.
Aftercare is a vital aspect of endodontic treatment to ensure a successful outcome. Patients are advised to follow proper oral hygiene practices, including brushing twice a day, flossing regularly, and scheduling routine dental check-ups. It is essential to avoid chewing on hard or sticky foods immediately after treatment to prevent any damage to the restored tooth.
Patients may experience mild discomfort or sensitivity after the